Despite technological progress, spine surgery remains high-risk for both surgeons and patients.
We're targeting the four critical areas where spine surgery fails both patients and the surgeons who treat them.
1
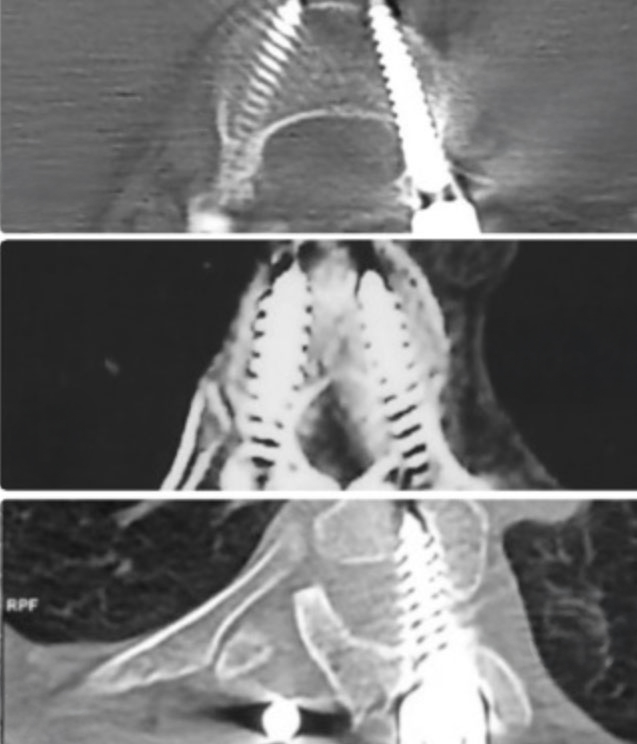
Pedicle screw malalignment
“Do no harm”
Sokrates
Of course, these never happen…
- Spinal cord injuries and neurological damage
- Major vascular perforations
- Mechanically unstable constructs
- Extended hospital stays and patient suffering
Freehand pedicle screw errors continue to cause avoidable complications and costly revisions – problems patients shouldn’t have to face.
- Veeravagu (2014) - Meta-analysis of pedicle screw complications in spine surgery
- Staartjes World Neurosurgery (2018) - Long-term outcomes of pedicle screw misplacement
- Bindels GSJ (2024) - Economic impact of revision spine surgery
>$2B
per year in extra expense globally
4-6%
of freehand surgeries require a revision
2
Excessive radiation exposure
Flooding the OR with X-rays and CT scans for screw checks is a dangerous and somewhat dated habit — putting surgeons, staff, and patients at needless risk of radiation damage.
Surely, there’s a smarter way…
- Cumulative exposure drives cancer, cataracts, thyroid disease
- Chronic radiation causes fatigue, impairs focus and clinical judgement
- Pediatric patients face higher lifetime risk
- Lead aprons are heavy, exhausting
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
Spine surgeons have a
greater cancer risk
Surgeons often exceed lifetime dose limits (e.g. hands, thyroid, whole‑body) even when annual levels appear compliant
Navigation and robotics shift radiation from surgeon to patient.
Intraoperative CT delivers 3–10× higher doses than fluoroscopy — hundreds of chest X-rays in one case.
Staff are safer, but patients, especially the young, face unnecessary long-term cancer risk.
3
Workflow interruptions
Surgeons face relentless pressure to operate faster, turn cases around quicker, and maximize OR throughput — yet every unnecessary delay makes that impossible.
Technology can increase workflow challenges…
- Wasting OR minutes – extends OR time and costs
- Frequent C-arm repositioning interrupts surgical workflow
- Navigation and robotics time-consuming setup wastes OR minutes
- One patient shift = full recalibration of CAS systems
- Veeravagu (2014) - Meta-analysis of pedicle screw complications in spine surgery
- Staartjes World Neurosurgery (2018) - Long-term outcomes of pedicle screw misplacement
- Bindels GSJ (2024) - Economic impact of revision spine surgery
OR Time Lost – Calculators
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
- Asari J. Orthop. Sci. (2022) - Radiation exposure risks in spine surgery
- Mastrangelo, Occ. Med. (2005) - Occupational cancer risk in surgical specialties
- Rampersaud et al. (2000) - Radiation exposure during spinal surgery
Wasted OR Time – Robot Setup
4–6
hours/month*
The equiavlent of 1-3 extra surgeries per month
* Drape, boot, register, plan, arm positioning (15-25mins) – 4 spine surgeries per week requring precision pedicle screw placement
4
Prohibitive Capital Investment Barriers
Navigation and Robotic systems reduce complication rates to between 0.7% and 0.9%; however, they require sizeable upfront investment, and have high annual maintenance costs.
It’s not all roses…
- Prohibitive capital + recurring costs*
- Hidden workflow tax
- Modest absolute risk reduction in many cases c.f. new smart instruments
- Surgeon autonomy & skill erosion
- Operational fragility & radiation trade-offs
* High purchase price, service contracts, disposables, and upgrade fees push the break-even point to very high volumes—creating a two-tier system where many hospitals simply can’t justify it.
- 2020 Millennium Research Group - Global spine device market analysis
- Biospace (2022) - Healthcare technology adoption barriers
- Grandview Research (2024) - Spine surgery market accessibility study